Member Spotlight: Chelle’s Story
Mental illness affects people just like me. Mental illness affects people different from me. You can’t just “snap out of it.” And it’s...
HOW WE TREAT OCD
Our providers understand the challenges of OCD, and have real-world experience helping people just like you.
Start with a free assessment
Our Care
Different people experience OCD in different ways. That’s why our providers work 1:1 with you to personalize treatment to your unique needs.
When medication is necessary, our psychiatric providers analyze 100+ data points to determine the most tolerable and effective prescription for you.
Our program combines cognitive and behavioral therapy with independent skill practice—all of which have been clinically proven to work for a wide range of symptoms.
Mental Health condition
People with OCD may have symptoms of obsessions, compulsions, or both. These symptoms can interfere with all aspects of life— such as work, school, and personal relationships.

Obsessive-compulsive disorder (OCD) is a common, chronic, and long-lasting disorder in which a person has uncontrollable, reoccurring thoughts (obsessions) and/or behaviors (compulsions) that they feel the urge to repeat over and over.
OCD affects up to 3% of people worldwide. Childhood onset can start around 10 years of age, more commonly in boys than girls. Most of the remainder of people with OCD have their first symptoms before they turn 25, with women outnumbering men. OCD symptoms don’t usually develop after age 30.

Obsessions are repeated thoughts, urges, or mental images that cause anxiety and fear.
Compulsions are repetitive behaviors that a person feels the urge to do in response to an obsessive thought.
HOW IT WORKS

Let your provider know how you’re feeling, get to know you, and provide 1:1 support.
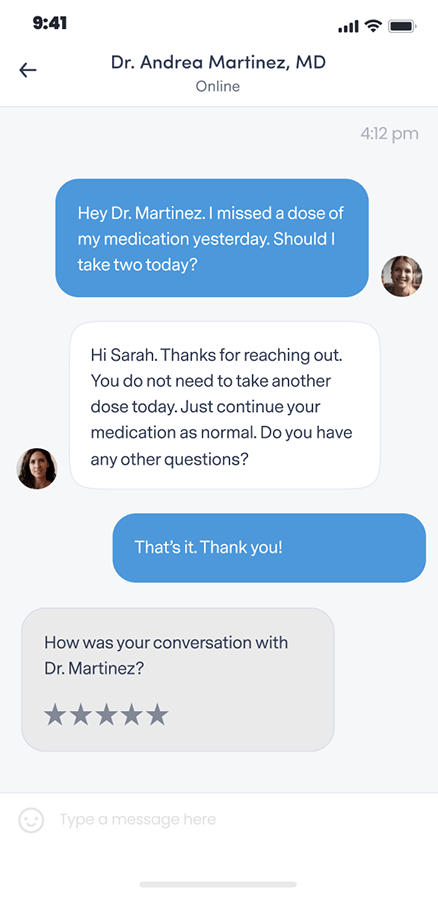
Get questions or concerns off your chest between video visits by messaging your provider at any time.
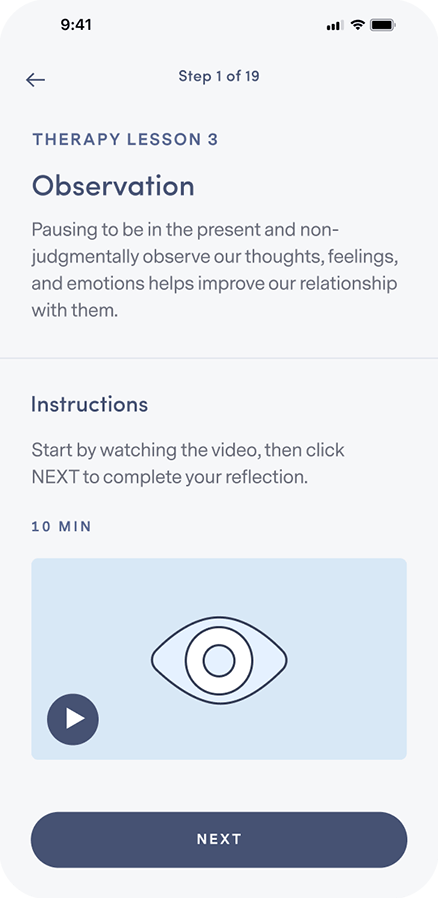
Learn how to integrate new thought and behavior patterns into your daily life.
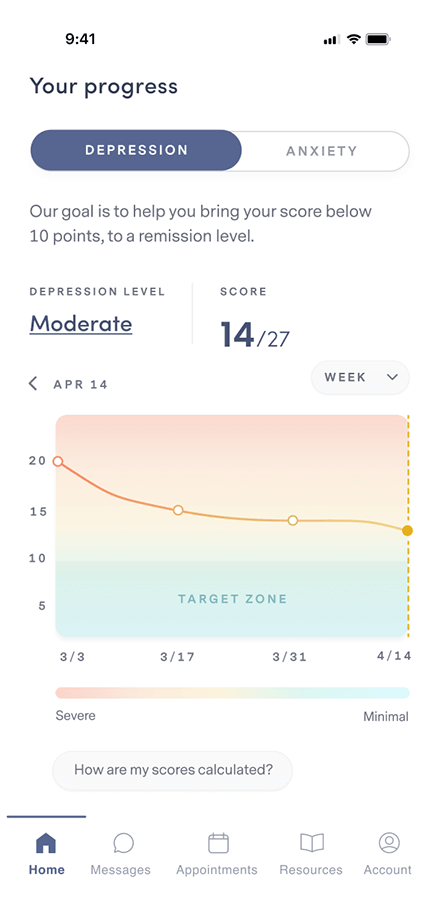
Complete weekly check-ins so your provider can track your progress and, if necessary, adjust your treatment and/or medication.
Our plan options
Because quality mental health care shouldn’t be out of reach for anyone.
PERSONALIZED
clinically-proven
comprehensive
Free Assessment
86% of our members feel better within 12 weeks.
We accept insurance.




FREQUENTLY ASKED QUESTIONS
If your question isn’t answered below, view our full list of FAQs here.
Brightside is available to people 18 years and older in the states where Brightside operates who believe they may be experiencing depression and may benefit from treatment.
Remote care is not a good fit for people with certain conditions or situations. These include (but are not limited to):
Our providers do not treat, and do not prescribe for adhd.
If any of these describe you, it’s best for you to be seen by a provider in person so you can get the care that’s right for you.
Brightside makes it easy to get top quality depression care from the privacy of home.
Here’s how Psychiatry works:
Here’s how Therapy works:
When scheduling your first appointment, you can browse all of our available providers in your state. Take a look at their profiles and check open times to find the best fit for you. Every Brightside provider undergoes a rigorous hiring and vetting process to ensure the highest quality care.
Brightside currently accepts select insurance plans in various states for payment of your provider’s or therapist’s services. Please see below for a current listing of plans. Brightside may not be included in all plans that each health insurance company offers. Please contact your health insurance plan to verify that your care at Brightside will be covered.
We currently accept the following insurance plans:
If you are a new member signing up for services you can enter your insurance information during the sign-up process. We’ll let you know your eligibility, as well as you estimated co-pays and out-of-pocket costs (if any) before signing-up or scheduling.
We also accept HSA/FSA payment if you have one of those accounts. If you have questions about using your medical or prescription insurance benefits, please contact us by emailing [email protected].
A mental health provider will diagnose OCD by asking you about the following three things:
The causes of OCD are unknown, but risk factors include:
Genetics
Twin and family studies have shown that people who have a parent, sibling, or child with OCD are at a higher risk for developing OCD themselves. The risk is higher if the first-degree relative developed OCD as a child or teen.
Brain structure
Brain imaging studies have shown differences in the frontal cortex and subcortical structures in patients with OCD. There appears to be a connection between the OCD symptoms and abnormalities in certain areas of the brain, but more research is needed to determine the specific connection.
Environment
An association between childhood trauma and OCD symptoms has been reported in some studies. However, more research is needed to understand this relationship better.
If you are experiencing obsessive thoughts and/or compulsive behaviors that are affecting your life, it may be time to seek professional help. Talk to your doctor about your symptoms and figure out a plan together.
OCD can be treated using a combination of medication and a few different therapy approaches.
Medication
Serotonin reuptake inhibitors (SRIs), including selective serotonin reuptake inhibitors (SSRIs), are used to help reduce OCD symptoms.
SRIs often require higher daily doses in the treatment of OCD than of depression and may take 8–12 weeks to start working. However, some patients do experience more rapid improvement.
Therapy
Certain types of therapy, including Cognitive Behavioral Therapy (CBT) and other related therapies (e.g. habit reversal training), can be as effective as medication for many people living with OCD.
Research also shows that a type of CBT called Exposure and Response Prevention (EX/RP) may also be helpful. EX/RP consists of spending time in the very situation that triggers the compulsions, such as touching a dirty object. Then, you won’t be allowed to complete the usual compulsion, such as handwashing. This type of CBT is effective in reducing compulsive behaviors in OCD, even in people who did not respond well to SRIs.
Self-Care, Coping, and Support
Many treatment plans for OCD involve aspects of self-care. This can include: