HOW WE TREAT INSOMNIA
Life-changing online care for insomnia
Our providers understand the challenges of insomnia, and have real-world experience helping people just like you.
Start with a free assessment
HOW WE TREAT INSOMNIA
Our providers understand the challenges of insomnia, and have real-world experience helping people just like you.
Start with a free assessment
Our Care
Different people experience insomnia in different ways. That’s why our providers work 1:1 with you to personalize treatment to your unique needs.
When medication is necessary, our psychiatric providers analyze 100+ data points to determine the most tolerable and effective prescription for you.
Our program combines cognitive and behavioral therapy with independent skill practice—all of which have been clinically proven to work for a wide range of symptoms.
Mental Health condition
People who experience insomnia typically report feeling unrefreshed when waking up, waking too early in the morning, or having trouble falling asleep at night.

Insomnia isn’t a lack of sleep now and then—it’s a real sleep disorder that affects millions of people. In fact, the APA estimates that six to eight percent of adults have symptoms severe enough for them to be diagnosed with insomnia disorder.
Insomnia and mental health are closely linked. Anxiety and depression can lead to insomnia, and insomnia can fuel the symptoms of anxiety and depression. This self-perpetuating cycle can lead to chronic insomnia.
Several anxiety and depressive disorders, such as Generalized Anxiety Disorder (GAD), panic disorder, and Major Depressive Disorder (MDD), can result in varying degrees of insomnia.

HOW IT WORKS

Let your provider know how you’re feeling, get to know you, and provide 1:1 support.
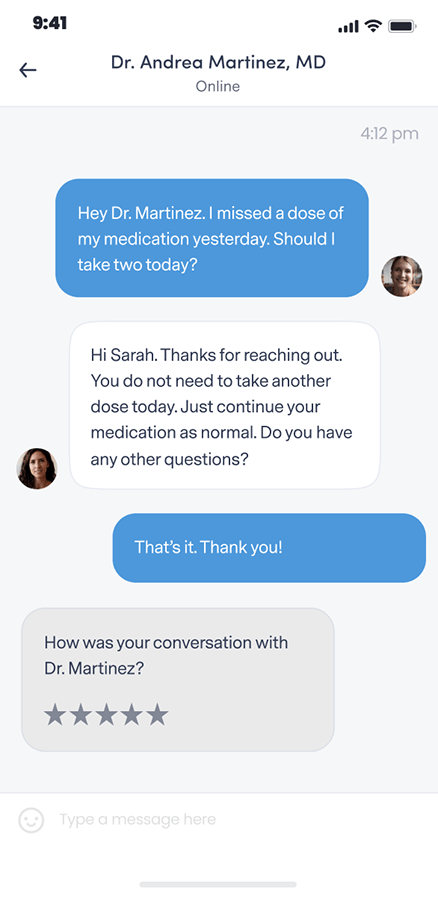
Get questions or concerns off your chest between video visits by messaging your provider at any time.
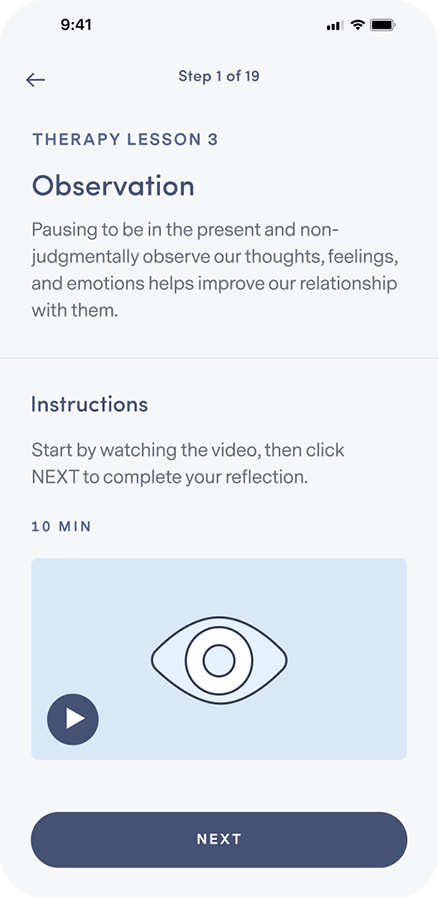
Learn how to integrate new thought and behavior patterns into your daily life.
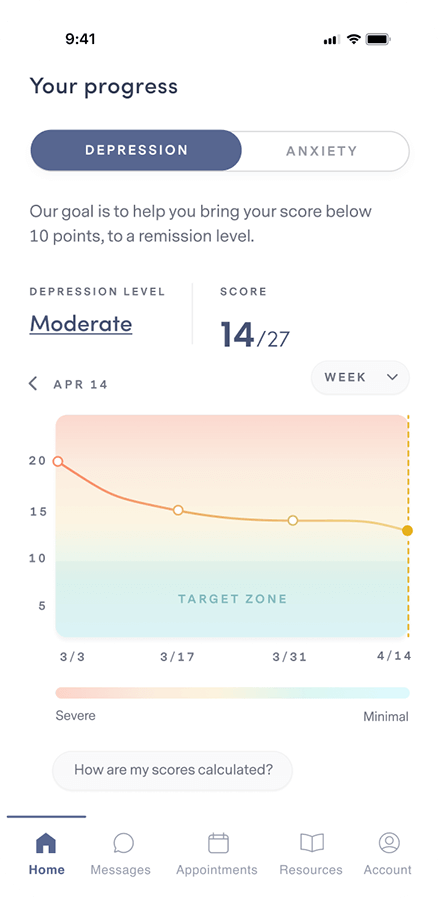
Complete weekly check-ins so your provider can track your progress and, if necessary, adjust your treatment and/or medication.
Our plan options
Because quality mental health care shouldn’t be out of reach for anyone.
PERSONALIZED
clinically-proven
comprehensive
Free Assessment
86% of our members feel better within 12 weeks.
We accept insurance.




FREQUENTLY ASKED QUESTIONS
If your question isn’t answered below, view our full list of FAQs here.
Brightside is available to people 18 years and older in the states where Brightside operates who believe they may be experiencing depression and may benefit from treatment.
Remote care is not a good fit for people with certain conditions or situations. These include (but are not limited to):
Our providers do not treat, and do not prescribe for adhd.
If any of these describe you, it’s best for you to be seen by a provider in person so you can get the care that’s right for you.
Brightside makes it easy to get top quality depression care from the privacy of home.
Here’s how Psychiatry works:
Here’s how Therapy works:
When scheduling your first appointment, you can browse all of our available providers in your state. Take a look at their profiles and check open times to find the best fit for you. Every Brightside provider undergoes a rigorous hiring and vetting process to ensure the highest quality care.
Brightside currently accepts select insurance plans in various states for payment of your provider’s or therapist’s services. Please see below for a current listing of plans. Brightside may not be included in all plans that each health insurance company offers. Please contact your health insurance plan to verify that your care at Brightside will be covered.
We currently accept the following insurance plans:
If you are a new member signing up for services you can enter your insurance information during the sign-up process. We’ll let you know your eligibility, as well as you estimated co-pays and out-of-pocket costs (if any) before signing-up or scheduling.
We also accept HSA/FSA payment if you have one of those accounts. If you have questions about using your medical or prescription insurance benefits, please contact us by emailing [email protected].
You may be diagnosed with insomnia if you have difficulty falling or staying asleep for at least three nights a week. Short-term insomnia lasts less than three months. Chronic insomnia lasts for three months or longer. Your doctor may do more tests to see whether your insomnia has caused any underlying health conditions.
Before seeing your doctor, it may be helpful to keep a sleep diary for one to two weeks. A sleep diary can help your doctor understand your sleep problem and whether certain activities or substances (like caffeine) are affecting your sleep. Write down when you go to sleep, wake up, and take naps each day. Also keep track of how sleepy you feel throughout the day, when you drink caffeine or alcohol, and when you exercise.
Worries can keep your mind active at night. Issues with work, school, family, and money can trigger your symptoms of anxiety. Not getting a good night’s sleep can further exacerbate feelings of anxiety.
Sleep problems affect more than 50% of adults with GAD. Researchers have discovered that sleep disruption—which affects levels of neurotransmitters and stress hormones, among other things—wreaks havoc in the brain, impairing thinking and emotional regulation. In this way, insomnia may amplify the effects of psychiatric disorders, and vice versa.
Studies estimate that 65% to 90% of adults with MDD experience some kind of sleep problem. Insomnia also increases the risk of developing depression.
A meta-analysis of 34 different studies concluded that poor sleep—especially during times of stress—significantly increased the risk of developing depression.
In another study, researchers found that as insomnia persisted, the subjects developed an even greater risk for depression.
Insomnia can occur at any age, but is more likely to affect women than men. Other risk factors for insomnia can include:
If you have trouble falling asleep, staying asleep, or don’t wake up feeling refreshed, it might be time for a conversation with your doctor. Untreated sleep problems can lead to a host of other problems and can set the stage for negative thinking and emotional vulnerability.
Cognitive Behavioral Therapy (CBT-I) can be helpful for people suffering from insomnia. Those with insomnia tend to become preoccupied with not falling asleep. CBT techniques can help you change negative expectations and build more confidence in having a good night’s sleep.
There are a handful of alternative treatments that can help insomnia, including lifestyle changes, better sleep hygiene, and relaxation techniques.
Lifestyle changes
Most people know that caffeine contributes to sleeplessness. But did you know that alcohol and nicotine can, too?
Alcohol initially depresses the nervous system, which can help some people fall asleep, but the effects wear off in a few hours and can cause unrestful sleep. Nicotine is a stimulant, which speeds heart rate and thinking and can inhibit the natural bodily processes for sleep.
Giving up these substances is best, but avoiding them before bedtime is another option.
Physical activity
Regular exercise can help you fall asleep faster, spend more time in deep sleep, and awaken less often during the night.
Sleep hygiene
Many experts believe that people “learn” insomnia, and can therefore “learn” how to sleep better. Good sleep hygiene is the term often used to include tips like maintaining a regular sleep-and-wake schedule. The idea is to use the bedroom only for sleeping and sex, and keep the bedroom dark and free of distractions like the computer or TV.
Some experts also recommend “sleep retraining,” which means staying awake longer in order to ensure sleep is more restful.
Relaxation techniques
Meditation, guided imagery, deep breathing exercises, and progressive muscle relaxation (alternately tensing and releasing muscles) can counter anxiety and racing thoughts.
Melatonin
Evidence suggests that melatonin is not effective in treating most primary sleep disorders with short‐term use, although there is some evidence to suggest that melatonin is effective in treating delayed sleep phase syndrome with short‐term use.
Evidence suggests that melatonin is not effective in treating most secondary sleep disorders with short‐term use.