HOW WE TREAT PPD
Life-changing online care for postpartum depression
Our providers understand the challenges of PPD, and have real-world experience helping people just like you.
Start with a free assessment
HOW WE TREAT PPD
Our providers understand the challenges of PPD, and have real-world experience helping people just like you.
Start with a free assessment
Having a hard time after giving birth? Take our short online postpartum depression test to find out if you’re living with postpartum depression.
Our Care
Different people experience PPD in different ways. That’s why our providers work 1:1 with you to personalize treatment to your unique needs.
When medication is necessary, our psychiatric providers analyze 100+ data points to determine the most tolerable and effective prescription for you.
Our program combines cognitive and behavioral therapy with independent skill practice—all of which have been clinically proven to work for a wide range of symptoms.
Mental Health condition
Over 50% of PPD cases go unrecognized. We want to work towards lowering that statistic by recognizing more cases using validated screening tools. PPD is a severe mental health issue and can manifest as feeling disconnected from your baby, feelings of intense sadness, or feeling incompetent as a mother.

The “baby blues” is a mild and common form of depression that can affect new mothers. Postpartum depression (PPD), however, is a more severe and debilitating condition affecting one in seven women. What is supposed to feel like a joyous time can actually cause feelings of apathy, anxiety, and sadness.
There are short- and long-term symptoms of PPD, and these symptoms may cause new mothers to feel isolated, guilty, or ashamed. PPD is one of the most significant causes of maternal morbidity and mortality. Risks of untreated PPD include suicide, feeling unhappy in your marriage, and even problems in your baby’s development. If you suspect that you might be suffering from PPD, do not suffer in silence or dismiss your struggles.

HOW IT WORKS

Let your provider know how you’re feeling, get to know you, and provide 1:1 support.
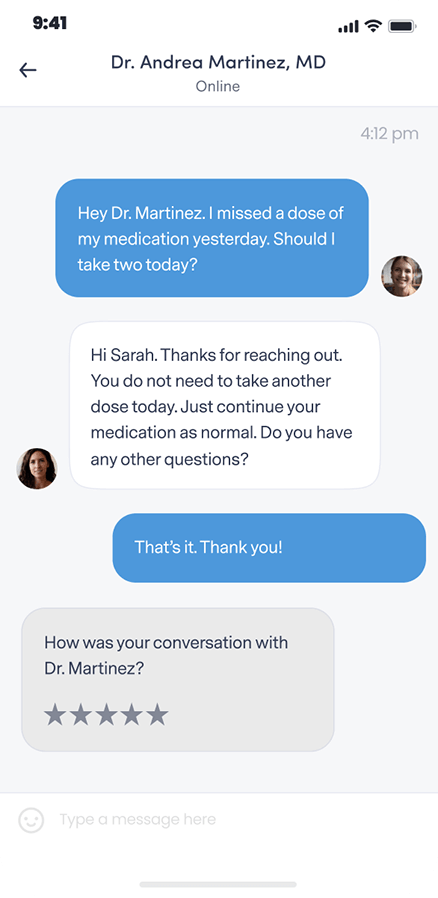
Get questions or concerns off your chest between video visits by messaging your provider at any time.
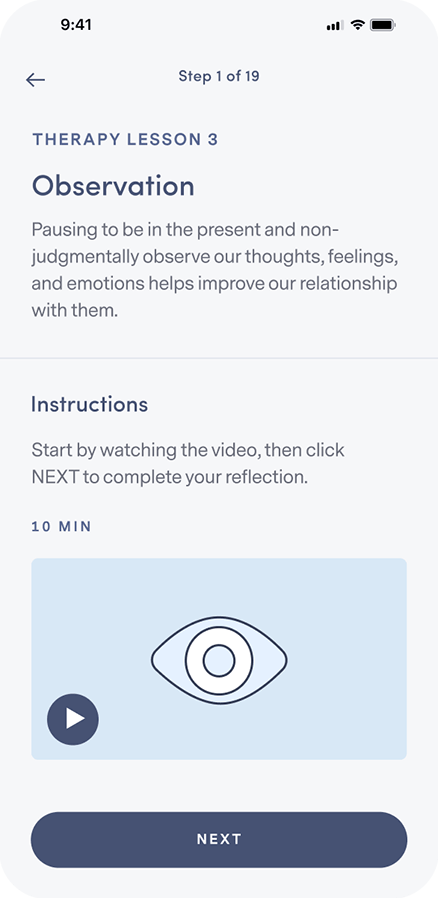
Learn how to integrate new thought and behavior patterns into your daily life.
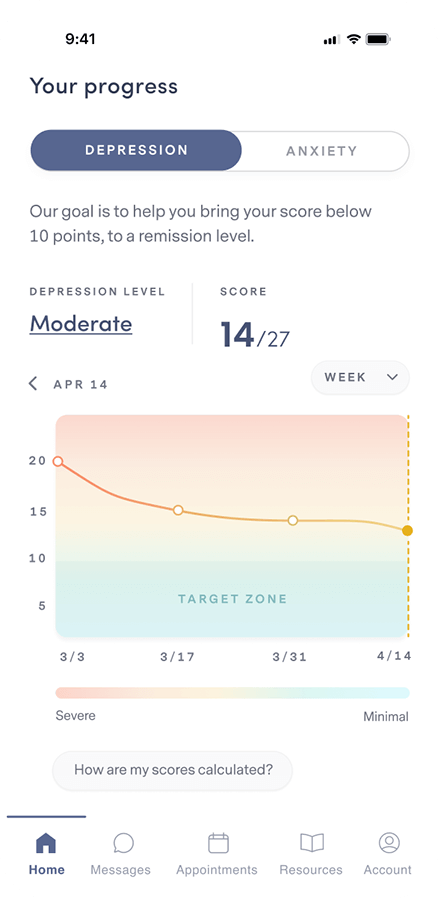
Complete weekly check-ins so your provider can track your progress and, if necessary, adjust your treatment and/or medication.
Our plan options
Because quality mental health care shouldn’t be out of reach for anyone.
PERSONALIZED
clinically-proven
comprehensive
Free Assessment
86% of our members feel better within 12 weeks.
We accept insurance.




FREQUENTLY ASKED QUESTIONS
If your question isn’t answered below, view our full list of FAQs here.
Brightside is available to people 18 years and older in the states where Brightside operates who believe they may be experiencing depression and may benefit from treatment.
Remote care is not a good fit for people with certain conditions or situations. These include (but are not limited to):
Our providers do not treat, and do not prescribe for adhd.
If any of these describe you, it’s best for you to be seen by a provider in person so you can get the care that’s right for you.
Brightside makes it easy to get top quality depression care from the privacy of home.
Here’s how Psychiatry works:
Here’s how Therapy works:
When scheduling your first appointment, you can browse all of our available providers in your state. Take a look at their profiles and check open times to find the best fit for you. Every Brightside provider undergoes a rigorous hiring and vetting process to ensure the highest quality care.
Brightside currently accepts select insurance plans in various states for payment of your provider’s or therapist’s services. Please see below for a current listing of plans. Brightside may not be included in all plans that each health insurance company offers. Please contact your health insurance plan to verify that your care at Brightside will be covered.
We currently accept the following insurance plans:
If you are a new member signing up for services you can enter your insurance information during the sign-up process. We’ll let you know your eligibility, as well as you estimated co-pays and out-of-pocket costs (if any) before signing-up or scheduling.
We also accept HSA/FSA payment if you have one of those accounts. If you have questions about using your medical or prescription insurance benefits, please contact us by emailing [email protected].
The specific cause of PPD is unknown, and any new mother can experience the symptoms. Those who are at risk of developing PPD include women who have previously experienced depression or who have a family history of depression.
Research has also shown that rapid changes in sex, stress, or thyroid hormones during and after delivery may contribute as well.
Other factors that may predispose you to PPD include:
In order to diagnose PPD, your healthcare provider may use a clinically-validated screening tool such as the Edinburgh Postnatal Depression Scale (EPDS). This questionnaire consists of a list of 10 short statements. For each statement, you’ll say how often you’ve felt that way in the past seven days. The higher the score on the screener, the more likely that you may be suffering from PPD.
There is hope. PPD is treatable, and with proper treatment, you’ll be back to feeling like yourself again. PPD can be treated both with medication and without.
Non-pharmacologic treatments for PPD include lifestyle changes, such as getting adequate sleep, proper nutrition, and plenty of exercise. Having a healthy social support system and getting your partner involved in your recovery is another treatment option. If you have the opportunity, ask friends, family, or your partner to take on additional responsibilities. This provides you time to exercise, time away from the baby, and time to get the sleep you need to recharge. Finally, getting connected with a therapist that specializes in cognitive behavioral therapy (CBT) has been shown to have great success in treating PPD without the use of medication.
If indicated, a doctor will prescribe medication to treat the symptoms of PPD. When you first seek treatment, it is essential to get your symptoms under control. This can take anywhere from six to twelve weeks and is known as the acute phase of treatment. Once your symptoms have normalized, your doctor will continue your medication therapy for four to nine months. This period is critical to ensuring lasting effects and is called the continuation phase of treatment. If you’ve had three prior episodes of depression or have a history of depression in your past, you may need to continue treatment for longer. Once your doctor is confident that your symptoms have waned, they will discontinue the medication by slowly weaning you off.
If you think you might be suffering from PPD, there is a clinically validated screening tool called the Edinburgh Postnatal Depression Scale (EPDS) you can take online to find out. This questionnaire is easy to take on your own and may bring clarity to your symptoms. This screening tool is a good exercise to start a conversation about PPD. It may be beneficial for all new moms to take (even in the third trimester of pregnancy before giving birth). A score higher than ten indicates possible PPD. If you score a ten or higher, we suggest making an appointment with your doctor to discuss treatment options.
If you know someone experiencing PPD, provide support whenever you can. Offer to take the baby for a few hours or set up a child-free get-together. Social support is vital for new moms suffering from PPD and can provide much-needed relief.