Member Spotlight: Chelle’s Story
Mental illness affects people just like me. Mental illness affects people different from me. You can’t just “snap out of it.” And it’s...
HOW WE TREAT PDD
Our providers understand the challenges of persistent depressive disorder, and have real-world experience helping people just like you.
Start with a free assessment
Our Care
Different people experience persistent depressive disorder in different ways. That’s why our providers work 1:1 with you to personalize treatment to your unique needs.
When medication is necessary, our psychiatric providers analyze 100+ data points to determine the most tolerable and effective prescription for you.
Our program combines cognitive and behavioral therapy with independent skill practice—all of which have been clinically proven to work for a wide range of symptoms.
Mental Health condition
The symptoms of persistent depressive disorder and major depressive disorder are similar. However, the main symptom of PDD is long-lasting low mood.

Persistent depressive disorder (PDD), formerly known as dysthymia, is a form of depression. The symptoms of PDD may be less severe than major depressive disorder (MDD), but they persist for longer periods of time.
While MDD is often episodic, PDD is more constant, sometimes lasting for years. For some people, the disorder starts during childhood, which can result in a person believing that depression is part of their character or personality.

HOW IT WORKS

Let your provider know how you’re feeling, get to know you, and provide 1:1 support.

Get questions or concerns off your chest between video visits by messaging your provider at any time.

Learn how to integrate new thought and behavior patterns into your daily life.
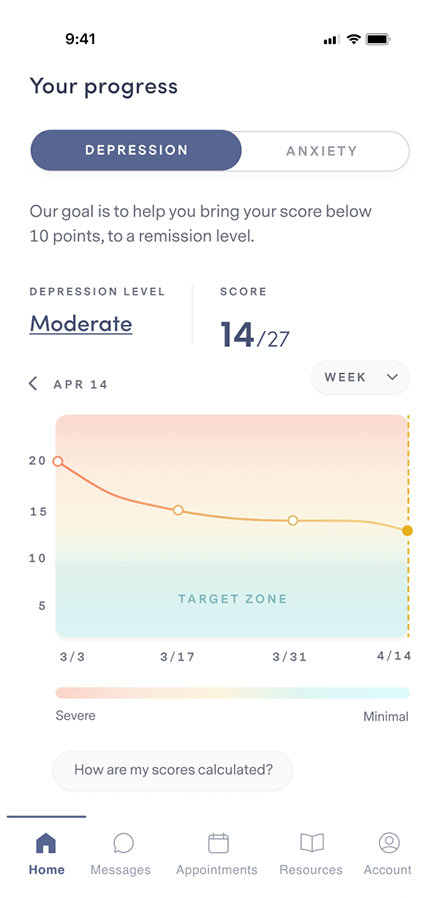
Complete weekly check-ins so your provider can track your progress and, if necessary, adjust your treatment and/or medication.
Our plan options
Because quality mental health care shouldn’t be out of reach for anyone.
PERSONALIZED
clinically-proven
comprehensive
Free Assessment
86% of our members feel better within 12 weeks.
We accept insurance.





FREQUENTLY ASKED QUESTIONS
If your question isn’t answered below, view our full list of FAQs here.
Brightside is available to people 18 years and older in the states where Brightside operates who believe they may be experiencing depression and may benefit from treatment.
Remote care is not a good fit for people with certain conditions or situations. These include (but are not limited to):
Our providers do not treat, and do not prescribe for adhd.
If any of these describe you, it’s best for you to be seen by a provider in person so you can get the care that’s right for you.
Brightside makes it easy to get top quality depression care from the privacy of home.
Here’s how Psychiatry works:
Here’s how Therapy works:
When scheduling your first appointment, you can browse all of our available providers in your state. Take a look at their profiles and check open times to find the best fit for you. Every Brightside provider undergoes a rigorous hiring and vetting process to ensure the highest quality care.
Brightside currently accepts select insurance plans in various states for payment of your provider’s or therapist’s services. Please see below for a current listing of plans. Brightside may not be included in all plans that each health insurance company offers. Please contact your health insurance plan to verify that your care at Brightside will be covered.
We currently accept the following insurance plans:
If you are a new member signing up for services you can enter your insurance information during the sign-up process. We’ll let you know your eligibility, as well as you estimated co-pays and out-of-pocket costs (if any) before signing-up or scheduling.
We also accept HSA/FSA payment if you have one of those accounts. If you have questions about using your medical or prescription insurance benefits, please contact us by emailing [email protected].
PDD is diagnosed when someone has been experiencing a depressed or low mood for two years or more. In addition to a persistent low mood, at least two of the following symptoms must be present: poor appetite or overeating, insomnia or hypersomnia, low energy/fatigue, low self-esteem, poor concentration/decision making, and hopelessness.
PDD can be diagnosed by a doctor or medical professional. The medical professional’s evaluation will identify specific symptoms and explore medical and familial histories as well as cultural and environmental factors. In some cases, lab testing and blood work might be done to make sure the depression is not due to a medical condition like a thyroid problem or a vitamin deficiency.
The reason why some people experience depression during their lifetime and others don’t is complicated, but it can be explained by utilizing the Biopsychosocial Model of Depression. The Biopsychosocial Model of Depression states that certain people are more vulnerable to developing depression because of biomedical and genetic risk factors, psychological risk factors, and societal, environmental, and social risk factors.
Biomedical & genetic risk factors
Certain physical illnesses, such as diabetes, cancer, heart disease, chronic pain, thyroid disease, and Parkinson’s disease can contribute to the onset of depression. Medications taken for these physical illnesses may also cause side effects that contribute to depression.
Further, some individuals have a genetic predisposition to developing depression. For example, if someone has a parent or sibling with major depression, that person has a two or three times greater risk of developing depression compared with someone who does not have depression in their immediate family members.
Psychological risk factors
Various aspects of how we automatically view the world, ourselves, and our relationships, may leave us to be vulnerable to developing depression. For example, a tendency to feel helpless when facing stressors in our life, having a natural tendency to ruminate about problems, having a negative perception of one’s self, the world, and the future, and having difficulty with relationships like feeling overly dependent on others, all can contribute to the development of depression.
Societal, environmental, & social risk factors
As human beings, we live in a society with others. Exposure to certain stressful situations throughout the lifespan can contribute to one’s vulnerability to develop depression. For example, people who experienced child maltreatment (physical abuse, sexual abuse, neglect, and/or emotional abuse) are at a much higher risk for developing depression as an adult. Some recent research indicates that this group of people are twice as likely to develop depression as an adult than those who did not experience any child maltreatment.
Living in poverty also makes people more vulnerable to depression. Those living in poverty are exposed to more violence and crime, and trauma, which all in turn also increase one’s risk for developing depression.
Stressful life events can also make people more likely to develop depression. For example, experiencing a pandemic, as we are now, chronic stress, or single major life events that are threatening and/or impact one’s personal goals and vision of their future. These could be events like losing one’s job or going through a divorce.
Protective factors
Certain personal characteristics, habits, and environments can help protect people at risk for depression from developing it. Some of these protective factors include:
It’s normal to feel sad or have days when you feel down. However, if you feel like a low or depressed mood has become your “normal,” it might be time to seek professional help.
The first step is to talk to a doctor or mental health professional about your symptoms. Symptoms of PDD may not improve on their own, so getting help is key to feeling better.
PDD can be treated with medication, therapy, or a combination of the two. There are also a variety of alternative treatment options that can help ease symptoms, such as supplements, although some may not be regulated by the FDA.
Medication
Medication is an effective form of depression treatment for many people. Because there are many forms of depression and each individual is unique, getting the best result requires matching each individual to the right medication. Then, once a treatment plan has been established, your doctor can fine-tune further treatment based on your response to the medication.
Medications commonly prescribed as a first line of treatment for depression include selective serotonin reuptake inhibitors (SSRIs) and norepinephrine-dopamine reuptake inhibitors (NDRIs). Common examples include Sertraline (Zoloft), Escitalopram (Lexapro) and Bupropion (Wellbutrin). There are other categories of medications that are used as well. Have a conversation with your doctor to figure out if medication is the right treatment option for you.
It typically takes at least two to six weeks of taking an antidepressant to see improvement. It may also take several trials to find the medication that works best. Once the right medication is found, dosage may be adjusted to optimize results.
We believe that everyone with depression should get specialized, expert care. This includes an experienced clinician taking the time to complete a comprehensive diagnostic evaluation, using data and clinical decision support to make an informed prescribing decision (if medication is appropriate), and practicing measurement-based care to monitor progress and adjust treatment accordingly.
Brightside offers medication plans to treat MDD. Click here to learn more about our medication plan offerings.
Therapy
Therapy may help alleviate some of the symptoms of depression by allowing you to:
Therapy can help you develop the skills you need to improve your depression. It can also be a helpful tool if depression is getting in the way of feeling your best and living the life you want.
If you’re ready to take the plunge into therapy, click here to get connected with our providers today.
Supplements
Research has shown that depression is influenced by a number of processes inside the body, including inflammation, oxidative stress, and more. Because of this, certain supplements have been used to help alleviate symptoms in people with depression for decades. However, the frontline treatment of depression is medication and/or therapy.
Fish oil (high EPA)
Fish oil is high in omega 3 fatty acids, which are key to certain brain functions and may help reduce inflammation associated with depression. There are two types of omega 3s in fish oil: EPA and DHA. Researchers found that EPA is the one that helps the most when it comes to depression.
Vitamin D
Our bodies produce vitamin D naturally with adequate exposure to the sun; however, studies have found that most people actually have insufficient levels, especially those living in northern latitudes with less sunlight exposure, and that people with low vitamin D levels are prone to higher rates of depression. There are vitamin D receptors in parts of the brain associated with depression and it may be involved in the creation of certain neurotransmitters.
L-Methylfolate (a specific type of folic acid)
Certain people have a genetic makeup that actually impairs their use of folic acid in cellular processes, which may be associated with depression. L-Methylfolate can help bridge this gap and keep the cellular processes moving. In fact, there is already an FDA-approved form of L-Methylfolate that doctors prescribe to patients who don’t initially respond to antidepressant treatment.
SAM-e (S-adenosylmethionine)
SAM-e is a prescription drug in Europe but is available over the counter in the U.S. It’s a natural substance present in every cell in the body and brain that plays a role in numerous cellular processes. SAM-e is believed to work by increasing levels of serotonin in the brain, creating a similar effect to antidepressant medication.
If you are considering supplements to help combat depression, it’s important to talk to a doctor about what is right for you. Some nutritional supplements are not FDA regulated and tests have consistently shown variable quality and purity across manufacturers.
Self-Care, Coping and Support
Many treatment plans for depression involve aspects of self-care. Getting regular exercise and good quality sleep can have a major effect on managing the symptoms of your depression. Practicing mindfulness, keeping a healthy and balanced diet, and connecting with loved ones or a support group are also highly impactful ways to aid in treating depression.